The Pitfalls of Creating Appointment Scheduling Apps for Healthcare
On the edge of the pandemic
COVID-19 completely disrupted the healthcare sector, as well as the majority of public services. With lockdowns and social distancing imposed worldwide, people are forced to stay at home to prevent the disease from spreading. Doctors have to resolve a growing number of emergency cases while responding to numerous daily requests.
In addition, many clinicians have been required to shift their regular activities to fighting the pandemic. Treatment of noncoronavirus patients has been suspended, including people with chronic diseases. Survivor Views reports that 51% out of all the survey participants experienced care delay or cancellation due to the coronavirus outbreak, while 25% of respondents had a treatment delay of more than two weeks.
The World Health Organization confirms this. Experts at the WHO also found that 53% out of 155 countries had to postpone care for hypertension treatment, 49% for treatment for diabetes and diabetes-related complications, 42% for cancer treatment, and 31% for cardiovascular emergencies.
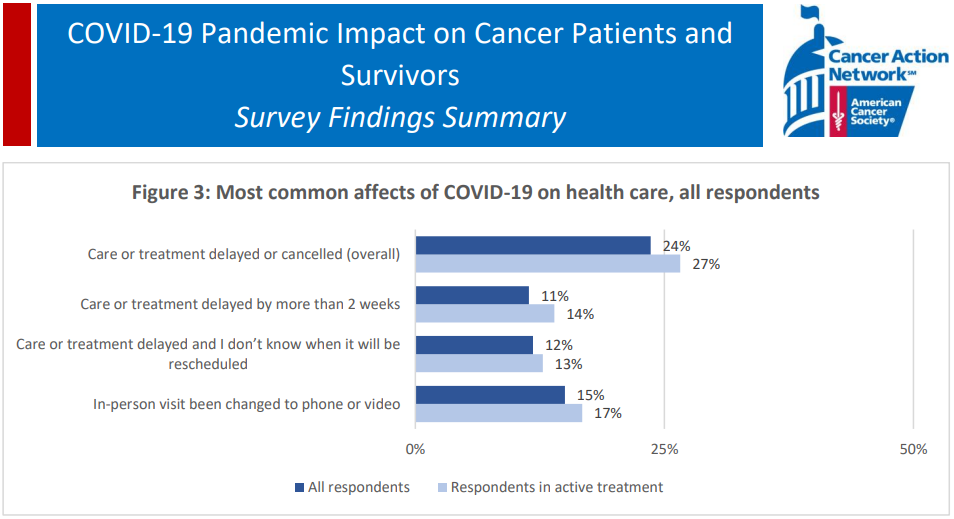 51% of patients experienced care delay or cancellation due to COVID-19 (Source)
51% of patients experienced care delay or cancellation due to COVID-19 (Source)As a result, The Guardian informs that over seven weeks from March 20 to April 24, there were extra 6,789 home deaths in England and Wales alone compared to the five-year average. Among these fatalities, just one out of four people died because of being infected with SARS-CoV-2, leaving 5,355 excess noncoronavirus deaths.
Similar situations were observed in other European countries, such as Spain (in spring) and Poland (in autumn).
In this context, healthcare companies are striving to:
- operate efficiently during the global pandemic, delivering services to both COVID-infected and noncoronavirus patients
- prevent the spread of COVID-19 by providing services in the safest way possible for both doctors and patients, aligning with social distancing protocols
- cope with the shortage of medical resources across all levels
According to analysis by the American Journal of Managed Care, patients spent 121 minutes at a doctor’s appointment on average, yet only 20 minutes with a healthcare professional, 37 minutes of travel time, and 64 minutes of waiting. As a consequence, a program capable of removing the need for commuting and for waiting in a queue could save patients over 100 minutes per visit. Having functionality for integrating health data with medical centers’ in-house systems, it may also save doctors and their assistants hours spent on paperwork weekly.
That’s why, since the beginning of the pandemic, the telemedicine sector skyrocketed and continues to grow faster than ever before. In the precoronavirus forecasts, the global telemedicine market was anticipated to reach $185.66 billion by 2026, increasing from $34.28 billion in 2018. Looks like the current situation will only accelerate this growth.
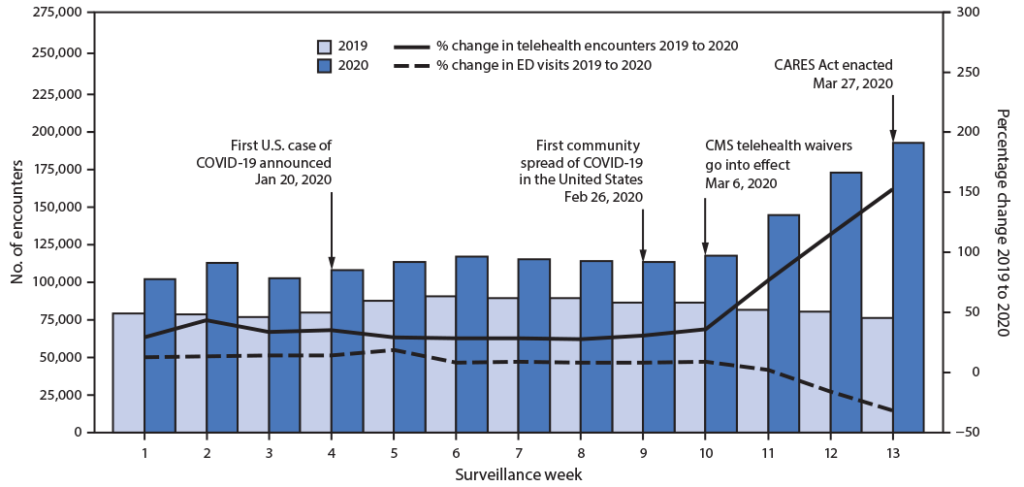 Spike in telehealth encounters starting from March 2020 (Source: CDC)
Spike in telehealth encounters starting from March 2020 (Source: CDC)This article describes what healthcare companies need to know when automating appointment scheduling, as well as how to address technical issues when building such a telemedicine app.
The components of an appointment scheduling app
In most cases, an online scheduling platform consists of both mobile and web clients. Since clinicians may work on desktops inside their institutions, the caregivers should be provided with rich dashboards helping to analyze patient history. A mobile app, in its turn, can enable patients to receive healthcare services at any moment and from any place in the world, as well as get timely reminders.
 An example of a virtual doctor app (Image credit)
An example of a virtual doctor app (Image credit)So, an appointment scheduling system сan include the following modules—from the high-level perspective.
- Video, audio, and text communication. With video and audio conferencing, healthcare professionals can give online consultations. Using chats, doctors and patients are able to share health data and treatment plans. In addition, a medical organization can incorporate an AI-based chatbot that will instantly answer frequently asked questions, offer tailored advice, and provide the requested information—for example, on healthy nutrition or coronavirus restrictions in the area. Thanks to notifications, it is possible to remind users about going to an appointment, taking medicines, and filling out a health-check questionnaire.
- Schedule management. The system should automatically check doctors’ working schedules, tailoring the time suitable for both sides in case any conflicts occur.
- Reporting. This allows healthcare experts to view medical information, the history of communication with patients, personal notes, etc.
- Health monitoring. This can be conducted either via questionnaires or sensors. For instance, people with diabetes should measure blood sugar level and share results with doctors everyday.
- An administration panel. Through such a module, healthcare companies can add new patients and doctors to the system, as well as manage roles.
- Billing management. An organization needs to allow patients to pay for medical procedures and consultations online. For this purpose, it can integrate a payment gateway, such as PayPal.
Many other components (e.g., doctor finder, location assistant, etc.) may also be included or be implemented as part of the modules described above. Let’s have a brief look under the hood.
Example #1. A sample architecture
Here’s an example of how Microsoft suggests building a microservices architecture for an abstract telehealth system like that.
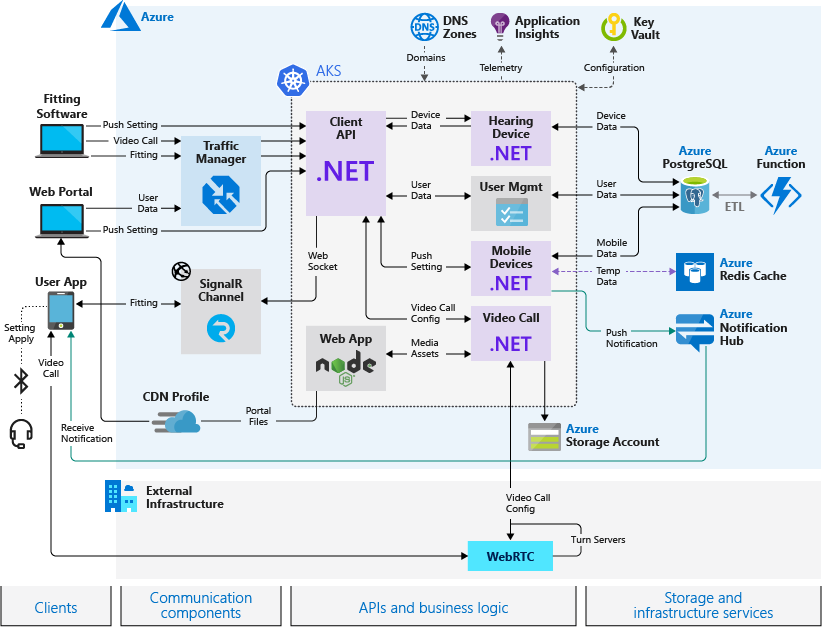 An architecture of an appointment system suggested by Microsoft (Image credit)
An architecture of an appointment system suggested by Microsoft (Image credit)In the proposed system, a web portal can be used to deliver services online, while patients can communicate via a mobile app. The architecture employs Azure Kubernetes Service for hosting the app’s business logic, facilitating deployment, and providing flexibility for customization. Other Azure services store medical data, as well as enable notifications, logging, balancing between multi-zone locations, video calls, etc. Depending on your app and care delivery processes, the workflow may differ.
Example #2. A sample communication tool
If an organization wants to build a chatbot for their telemedicine app, many solutions from Amazon may also help. For instance, aiming to help caregivers deliver healthcare services online, the company created an SMS chatbot for medical centers and hospitals. This product allows for escalating to a nursing phone line in case of health deterioration, while clinicians can include patients into specific treatment programs.
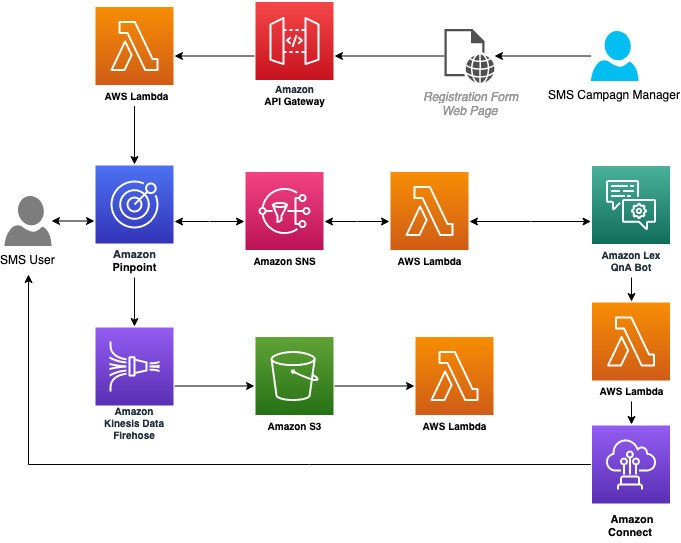 AWS resources required for building a chatbot (Image credit)
AWS resources required for building a chatbot (Image credit)Check out this tutorial for details.
Things to keep in mind
When building a system for appointment scheduling, development teams will inevitably encounter the following critical challenges.
- High availability, scalability, and performance. Availability of healthcare systems are crucial to delivering timely service, since in case of a failure patient lives are at stake. The same goes with scalability and performance. The systems should seamlessly scale on demand in accordance with growing loads, as well as operate uninterruptedly. System upgrades must not affect neither availability, nor performance.
- Contradicting schedules and no-shows. There are all sorts of unexpected and planned events that complicate shaping the clinic’s schedule—for instance, doctors’ days off and sick leaves. The COVID-19 pandemic contributed to the challenge with doctors being transferred to other departments/hospitals to help out their colleagues. A patient may have a force majeure, as well. Medical Group Management Association (MGMA) reports a median of 5% patient no-shows, with several specialties experiencing even higher rates. These missed appointments cost the global healthcare sector billions of dollars annually (£216 million pounds in the UK alone) and millions of wasted medical hours. All these things have to be taken into account while arranging a working schedule.
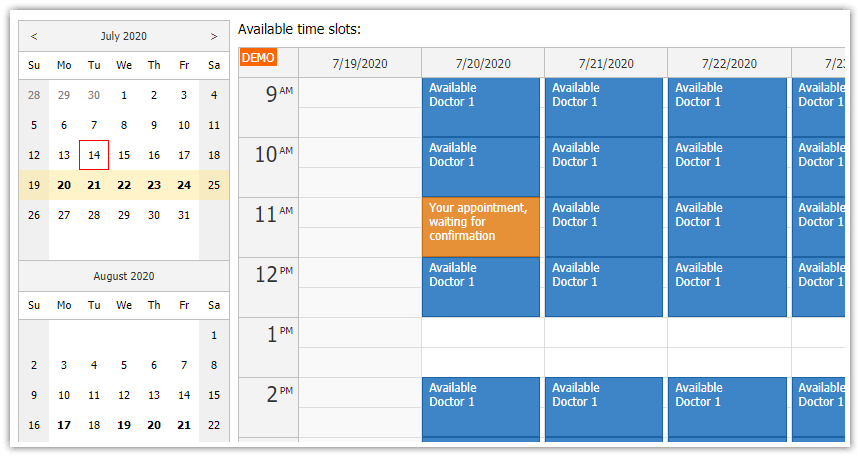 A sample doctor’s timetable (Image credit)
A sample doctor’s timetable (Image credit) - Integration. With a variety of medical data sources—many being unstructured or semi-structured—having a unified view of a patient’s medical history (including other necessary details) is not an easy task. This may lead to the need of integrating numerous internal systems (medical, financial, reporting, CRMs, etc.) and third-party ones (e.g., insurance) in a trusted, secure manner.
- Data privacy and security. Medical institutions are obliged to comply with certain regulations when dealing with personal data (e.g., GDPR in the European Union and HIPAA in the US).
- Adoption. The learning curve should be minimized as much as possible to facilitate adoption. Otherwise, the app will fail to meet its goals. Things like managing personal doctor data should nor require a separate engineer for this activity.
This brief list is by no means a comprehensive one. (Feel free to add your variants in the comments.) However, these issues will occur in most appointment scheduling apps.
How to address?
Ensuring high availability and scalability
Thoroughly thought-out architecture is halfway to success. A microservices-based architecture representing the unity of independent components, for instance, favors not only high availability and scalability, but also maintainability. Unlike monoliths, microservices allow for dealing with a particular component sparing the need to refactor the whole system.
For infrastructure, you may opt for ready-made platforms by Microsoft, Amazon, Google, or other established companies—fine-tuned specifically for the needs of healthcare. Multi-AZ infrastructures/data centers and content delivery networks (CDN) will further contribute to improving performance and minimizing response times.
To ensure zero-downtime upgrades, consider implementing a continuous integration/delivery pipeline by using tools for automating deployments (e.g., Jenkins or Concourse) and approaches such as blue-green deployment. For the sake of stability and automation of operations, Kubernetes distributions can also help.
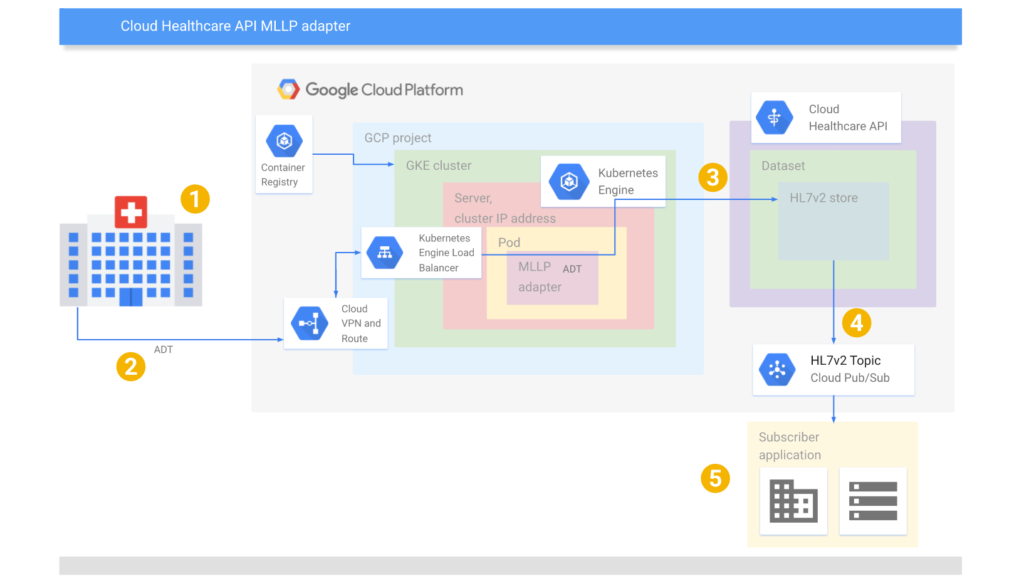 Using Google Kubernetes Engine and MLLP adapter for transmitting HL7v2 messages
Using Google Kubernetes Engine and MLLP adapter for transmitting HL7v2 messages(Image credit)
When improving scalability, explore NoSQL databases (which can be provided “as a service” within the IaaS platforms mentioned above), pay attention to load balancing, find performance bottlenecks, etc. In general, this topic—just like other issues here above and below—worth a separate book.
Optimizing conflicting schedules
One of the ways to address this is using artificial intelligence to build algorithms that will efficiently address the gaps in the doctor’s schedule. (Or, at least, develop some kind of decision trees to identify and avoid overlapping.) This may incude a variety of approaches—from optimizing appointment arrangements (for achieving maximum utilization) to additional double-booking in case the probability of cancellation is high enough. This paper and this article may help, to some extent.
Another right thing to do is enabling automated notifications (push, e-mail, and SMS) in case any arrangements change. Patients will also appreciate a direct link right in their inbox—leading to a schedule where a patient can choose an alternative time slot in case the doctor is on vacation, sick leave, etc.
Automatic appointment reminders and confirmations can also increase attendance.
“If we don’t have contact information for a patient and don’t try to contact them, our no-show rate is more than 10%. If we remind them of the appointment, the no-show rate drops to about 6%. However, if we ask them to confirm the appointment (touchtone, click, etc.), the no-show rate drops to less than 3%.” —Jeffrey Rydburg, MGMA
Integration and unification
Many enterprise systems have mature API tooling to serve the integration needs, as well as provide some functionality to extract, share, or even synchronize data. However, in many cases, this may not be enough. A customly developed in-house system may lack an API at all, so the need for developing it may arise at some point.
 A variety of sources for medical data formats (Image credit)
A variety of sources for medical data formats (Image credit)Nevertheless, when binding the apps together, introducing ETL/data quality initiatives will help to prevent transfer of duplicated or outdated information between the integrated systems. Compatibility of data may be improved by putting electronic health records (EHR) on the agenda. Solutions like Amazon HealthLake and Google’s Cloud Healthcare API can also assist in unifying, enhancing, and sharing medical data.
When integrating with insurance systems, it is worth exploring how blockchain can help. Relying on a system integrator with a proven track record in the field may accelerate the process, as well.
Compliance and security
In accordance with data privacy regulations, patient information has to be protected from unauthorized access, viruses, malware, mishandling, etc. Transparent and comprehensible privacy policies should be introduced notifying users about how their data is gathered, processed, and stored. To gather personal data aligning with GDPR, healthcare companies have to receive explicit consent from users and grant them the right to withdraw it at any time.
Medical organizations should be aware of any security risks their systems may be prone to and implement preventive measures: data encryption, role-based access control, two-factor authorization, regular audits of hardware and software, etc.
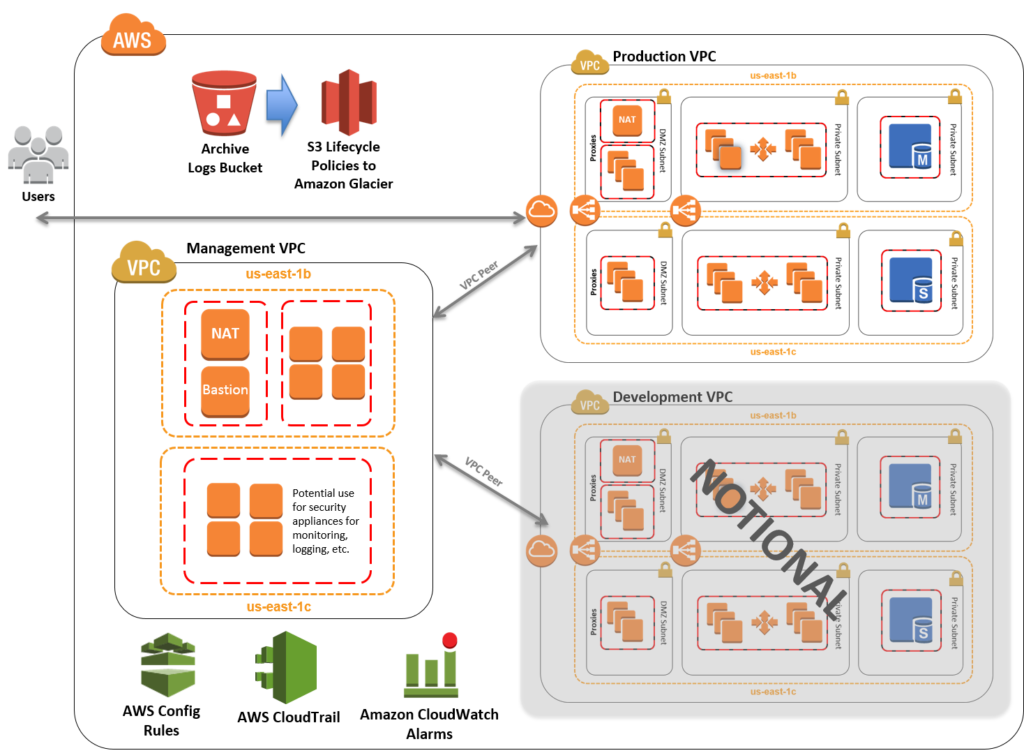 A HIPAA-compliant infrastructure suggested by Amazon (Image credit)
A HIPAA-compliant infrastructure suggested by Amazon (Image credit)Infrastructure vendors, such as Amazon, offer cloud deployments satisfying the requirements of HIPAA, HITECH, and other healthcare regulations. This may include creating an automatically configured environment containing security-focused components and features, such as identity and access management, virtual private clouds, multi-AZ services, SSH, logging/monitoring, etc.
Easing the learning curve
It is important to ensure that medical workers with no technical background could easily manage tasks such as addition of new doctors, their vacations or sick leaves, etc. Therefore, it makes sense creating a module that will enable easy management of user accounts—built for nontechnical users. Investing in training, how-tos, and documentation may also foster adoption. Kaiser Family Foundation suggests that the improvement of existing models and workflows can help to overcome adoption barriers, too.
Overall, before launching your product to public, you can make it available for a pilot group of users first—to gather early feedback and fix the most critical issues on the go.
The growing trend
Despite the additional budget needed, medical organizations can continue delivering their services during the pandemic by implementing telehealth solutions. Thanks to online appointments, for instance, it is easier to maintain the practice of social distancing to prevent the disease from spreading. According to the June 2020 survey by the National Association of Community Health Centers, 45% of visits to health centers in Pennsylvania were already conducted online.
To enable this, an effort is required from the medical institutions. This may include investment in IT infrastructure (such as broadband) to ensure smooth contact between a doctor and a patient during a remote session; adapting workflows to new models of delivering care/treatment; as well as updating insurance policies to cover telehealth services, probably. All these things should be evaluated against the expected automation (saved doctors’ time), increased service accessibility, etc.—to understand ROI and the budgets available.
Still, if implemented properly, telemedicine tools can improve the productivity of healthcare professionals, enabling to resolve more requests and emergency cases per day, as well as reduce paperwork. Patients could also save up to 2 hours per each visit, while minimizing the risk of getting infected on the way to a clinic or when waiting in hospital queues.
To learn more about how telemedicine and health information technology can improve patient treatment, download our research paper on the topic.
Further reading
- What’s Wrong with AI Tools and Devices Preventing COVID-19?
- Building a Mission-Critical Architecture for Healthcare with Cloud Foundry
- 15 Ways Telemedicine and Health Information Technology Can Improve Patient Care
edited by Sophia Turol.